Tissue grafts are widely used in medical procedures, from reconstructive surgery and orthopedics to dental applications and wound care. Despite their common use, not all grafts are the same. They can vary in origin, structure, processing, and intended function. To ensure clarity across medical, scientific, and regulatory environments, these grafts are grouped based on shared characteristics.
Understanding how tissue grafts are classified helps support proper use, storage, labeling, and communication across different sectors of the healthcare industry.
Source-Based Classifications
The first major way tissue grafts are categorized is by where they come from. This distinction matters not just for medical reasons, but also for how the material is screened and handled.
Autografts
An autograft comes from the patient’s own body. Since the donor and recipient are the same person, there’s typically less risk of immune rejection. These grafts are often used in procedures like bone or skin reconstruction.
Allografts
Allografts are donated by another person of the same species. The donor and recipient are not genetically identical, so these grafts require careful screening and preparation to reduce the risk of disease transmission or immune response.
Xenografts
Xenografts are taken from a different species, commonly pigs or cows. They are usually processed to remove cells and other materials that could trigger an immune reaction. These types of grafts may be used temporarily or in highly specialized procedures.
Isografts
Isografts are used between genetically identical individuals, such as identical twins. Because their genetic material matches, the body is less likely to reject the tissue.
Structure and Function
Another way to classify tissue grafts is based on what they are made of and how they function in the body.
Some grafts serve a structural purpose, like supporting bone or soft tissue. Others are designed to help cells grow or regenerate new tissue. Here are a few key terms used to describe this:
- Osteoconductive grafts provide a physical framework where bone can grow.
- Osteoinductive grafts have properties that stimulate cells to become bone-forming cells.
- Osteogenic grafts contain living cells that are already capable of building new bone.
In other types of grafts, like skin, nerve, or soft tissue, classification may depend on how well the graft supports healing, revascularization, or integration with the recipient’s body.
Processing and Handling Methods
Once tissue has been recovered, how it is handled also affects how it is classified. Processing can influence how long a graft lasts, how it should be stored, and how it performs in a surgical setting.
Fresh, frozen, or lyophilized (freeze-dried) grafts each have different handling requirements. Fresh grafts may retain more biological activity but have a shorter shelf life. Frozen and freeze-dried versions are easier to store and transport, though they may have different mechanical or biological properties.
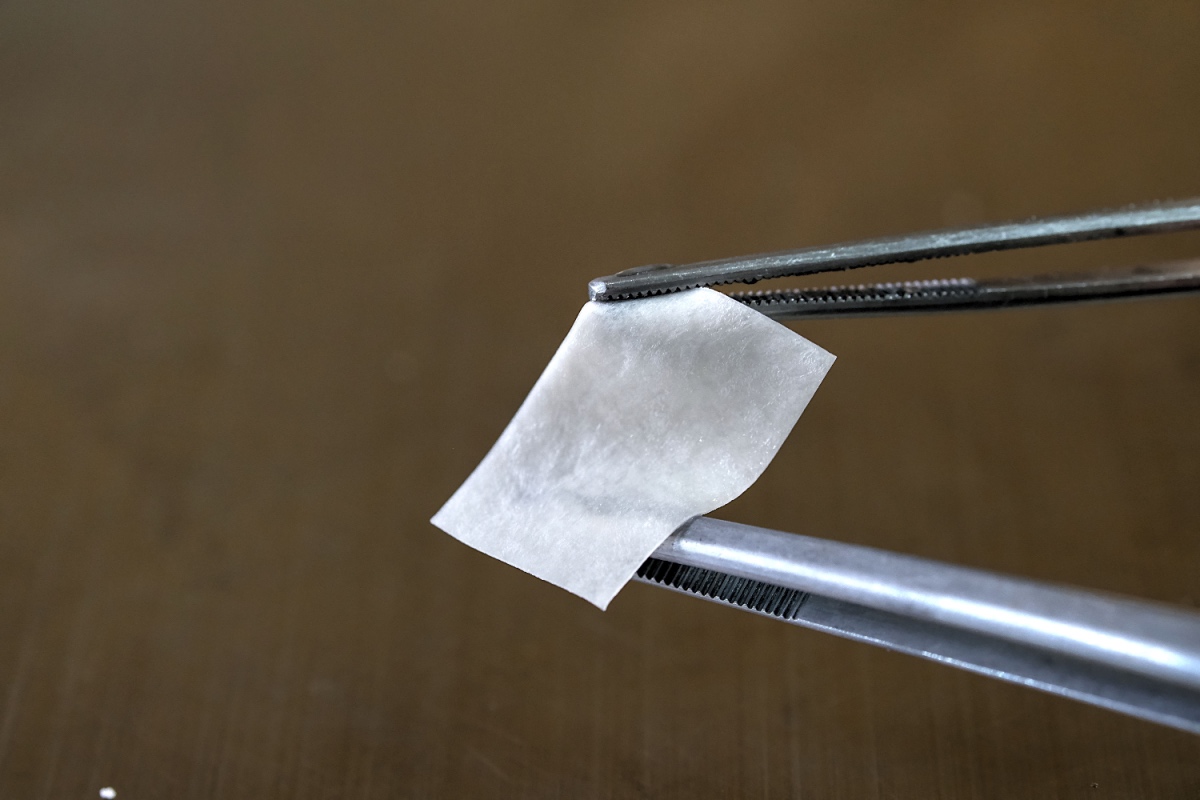
Some grafts are decellularized, meaning cells are removed to reduce the risk of rejection while preserving the underlying structure. This process is common in soft tissue grafts and matrices used in reconstructive procedures.
The amount of manipulation a graft undergoes during processing may also influence how it’s regulated. Minimal manipulation typically refers to changes that don’t alter the tissue’s original function. More extensive changes could place the product into a different regulatory category, depending on how it’s intended to be used.
Why Classification Systems Matter
These classifications help establish shared understanding between surgeons, manufacturers, researchers, and regulators. Standard terms provide clarity when ordering, documenting, and evaluating graft performance. They also support traceability, safety, and compliance with established regulations.
In clinical settings, classification helps guide surgical choices. In manufacturing and processing environments, it influences how tissue is labeled, stored, and validated. And in research and development, it offers a framework for comparing outcomes and improving future technologies.
Understanding Classification to Support Responsible Use
Tissue graft classification provides a shared language for understanding how different materials are sourced, processed, and applied. While clinical use may vary, the categories themselves offer a foundation for safer handling, clearer communication, and informed decision-making.
As the field of tissue-based products continues to grow, having a solid understanding of graft types and classifications helps support better outcomes across the board.
To learn more about Acesso Biologics and our products, get in touch with our team today.
Sources: